Abstract
Adults with atopic dermatitis (AD) have an increased risk for thromboembolic events. While coagulation is critical for almost all healing responses, dysregulated clotting and fibrin(ogen) deposition lead to inflammation that exacerbates tissue damage and impairs tissue repair. While plasma fibrin(ogen) has been associated with established asthma, fibrin(ogen)'s mechanistic role in AD pathogenesis and allergic sensitization has not been investigated. Here we show that fibrinogen plays a critical role in a murine model atopic dermatitis pathogenesis by markedly attenuating disease severity, barrier dysfunction, and allergic sensitization.
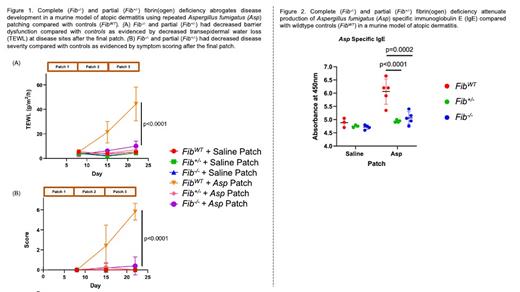
To determine if fibrinogen impacts AD pathogenesis, we used mice with complete fibrinogen deficiency (Fib -/-), partial deficiency (Fib +/-), and wildtype controls (Fib WT) in our established model of AD. This model uses repeated cutaneous allergen sensitization with heat-killed Aspergillus fumigatus (Asp) extract. Notably, Fib +/- mice produce approximately half as much fibrinogen as Fib WT mice. After each patch and at sacrifice each mouse underwent an objective disease severity assessment as well as transepidermal water loss (TEWL) measurements to assess skin barrier function. Our results show that complete and partial fibrinogen deficiency abrogated AD development. We found that Fib -/-and Fib +/- mice had markedly attenuated TEWL (P-value <0.0001) and disease severity (P-value <0.0001) compared with controls (Figure 1). In addition, we found that the TEWL and disease severity in Fib -/- and Fib +/- were comparable to unchallenged controls. There was also no difference in either outcome between Fib -/- and Fib +/- mice within the experimental group. Lastly, none of the Fib -/- and Fib +/- mice developed spontaneous bleeding.
Next, to elucidate the impact of fibrinogen on allergic sensitization we measured plasma allergen specific immunoglobulin E (sIgE) to Asp in all mice in our AD model at sacrifice. We found that Fib -/- and Fib +/- mice had significantly lower Asp sIgE compared with controls (p-value <0.0001 and 0.0002, respectively; Figure 2). In addition, we found that the amount of sIgE to Asp produced was comparable between Fib -/- and Fib +/- mice as well as with unchallenged controls.
Thus, our findings suggest that fibrin(ogen) plays a critical mechanistic role in driving AD development and allergic sensitization. While fibrinogen's role in established allergic disease has been shown, these novel findings suggest a critical role for fibrinogen in allergic disease pathogenesis which may allow for additional therapeutic targets to treat atopic dermatitis and other allergic diseases.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal